TEST NOW, ASSESSING YOUR RISK IS SIMPLE
HOW TO TEST
Genetic testing is easy and affordable. You can order a test from Color Health through Yodeah, and mail in a saliva test from home. Color Health, a clinical-grade genomics lab, has partnered with the American Cancer Society to promote cancer screenings and is a HIPAA-covered entity that follows all HIPAA privacy and security risks for safeguarding protected health information (PHI).
We encourage you to read the Know Before You Test section on this page.
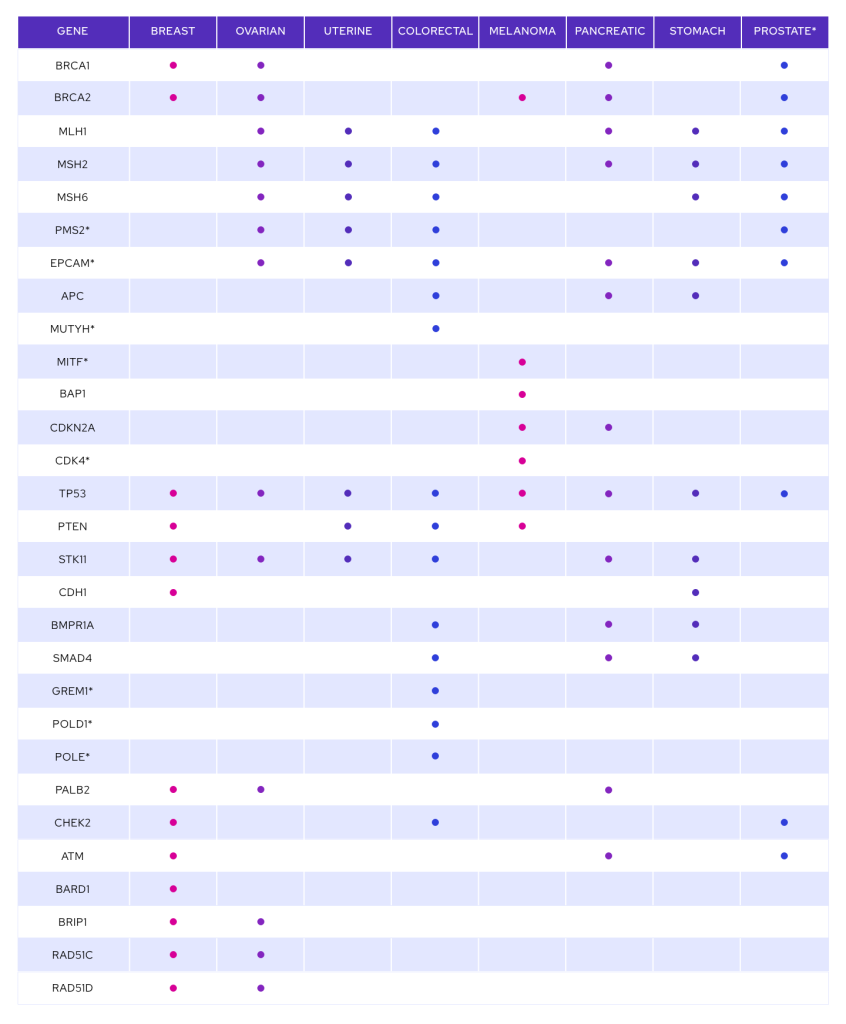
Click here for the list of genes included in the Color Health test.
ENTER OUR CODE KNOW30 AT CHECKOUT AND THE COST WILL CHANGE FROM $299 TO YODEAH'S DISCOUNTED RATE OF $149.
You can also test through your doctor's office or a genetic counselor.
WHAT TO KNOW BEFORE YOU TEST
BEFORE TESTING
Some information you should KNOW before you test:
- This test is for cancer susceptibility gene mutations, not for cancer itself. Even if you carry a genetic mutation, such as those found on the BRCA gene, it does not mean you will develop cancer; however, your risks for certain cancers are increased. If you are identified as having a hereditary cancer genetic mutation, lifesaving management guidelines can be implemented, including increased screening, medication, and medical procedures to prevent cancer.
- The one in 40 statistic applies to three specific genetic mutations on BRCA genes, called Ashkenazi Jewish founder mutations. Founder mutations account for the majority, but not all, of the BRCA mutations found in Ashkenazi Jews.
- The lab Yodeah uses screens for mutations on many cancer susceptibility genes, including all BRCA mutations, not just founder mutations. All mutations included in this test are actionable, meaning there are lifesaving options to reduce your risk of developing cancer.
- Yodeah recommends using only clinical-grade genomics labs for testing, not recreational genetic tests, which may not offer testing for all known mutations of BRCA genes or be a HIPAA-covered entity.
- Age to screen: guidelines do not recommend testing for a BRCA genetic mutation until age 18-25 unless there is a personal or family history of cancer at a younger age. This is in part because recommended management, such as increased screening for BRCA-associated cancers, doesn’t begin until age 25. However, if there is a personal or family history of cancer at a younger age or pediatric cancer, different recommendations exist, and full genetic counseling would be recommended.
- Your results should be put into the context of your personal and family history. What this means is that if your results are negative and you have a family history of cancer, your doctor may still suggest following you more closely with enhanced screening.
- Most cancers are sporadic, meaning unrelated to a hereditary gene like BRCA. It is important to continue appropriate cancer screening per medical guidelines.
Prior to testing, we encourage you to review the information below regarding the potential impact on your insurance.
- The Genetic Information Nondiscrimination Act (GINA): In 2008, a federal law was enacted called The Genetic Information Nondiscrimination Act (GINA), which prevents health insurance companies from discriminating against individuals who carry genetic mutations, such as those on the BRCA genes. This law has more limited protections for the military. GINA does not cover life, disability, or long-term care insurance. State laws regulate these types of insurance, and the laws vary from state to state. Please review your state law. You may want to consider having these policies in place prior to genetic testing. For additional information about GINA, please visit the National Human Genome Research Institute at https://www.genome.gov/about-genomics/policy-issues/Genetic-Discrimination.*
- Florida – Florida enacted a law that prohibits health insurers, life insurers and long-term care insurers from canceling, limiting, denying coverage or adjusting premium rates based on genetic information, unless there is a diagnosis of a condition related to the genetic information. There are, however, exceptions for other types of coverage. Life and long-term care insurers are still able to access a person’s medical record as part of an application exam and consider a medical diagnosis included in a medical record, even if based on the results of a genetic test.Health insurers, life insurers, long-term care insurers are also prohibited from requiring or soliciting genetic information, using genetic test results, or considering a person’s decision regarding genetic testing for insurance purposes.
- Please see Florida Statutes Section 627.4301 for additional information.
* The statements made herein are for informational purposes only and do not constitute legal advice.
This information is for guidance only. It is not meant to give specific medical advice. Always consult your healthcare provider.
AFTER TESTING
You gave your sample — now what?
Once the lab receives your saliva sample, they will keep you informed on the testing process through email or text. They may also send emails reminding you to fill out your personal and family history. This helps the lab put your results into context. The genetic results usually come back within 4-6 weeks, and the lab will contact you through phone calls or email. Because of health privacy laws, Yodeah does not receive your identified results, but we are available and happy to help guide you through the process.
Your results will fall into one of three different categories:
Negative: You do not carry a known pathogenic mutation/variant. This means that you do not carry a known hereditary cancer genetic mutation that can markedly increase your risk of some cancers. This is good news, but because most cancers are sporadic, meaning not associated with a hereditary cancer gene, you need to continue appropriate cancer screenings based on your age, family history, and other factors. For example, if this genetic testing is negative and you have no family history of breast cancer, the American College of Obstetrics and Gynecology currently recommends yearly mammograms beginning at age 40. However, if your genetic testing is negative but you have a strong family history of breast cancer, your doctor might recommend additional surveillance, such as adding yearly breast MRIs to your yearly mammograms or even medication to prevent breast cancer. Or if you have a family history of breast cancer at a younger age, your doctor might recommend beginning screening earlier than age 40. Your doctor can help put this into context for you.
Positive: You carry a pathogenic genetic mutation/variant that is associated with an increased risk of cancer. This does not mean you have or will have cancer. However, this information allows you to establish a personalized medical plan with a physician or genetic counselor. You can discuss medication and procedures to decrease your risk of cancer or enhanced surveillance to diagnose cancer at its earliest, most treatable stage. We also recommend testing your family members to see if they have the same mutation. Finally, if you are planning a family, you can discuss options, including in-vitro fertilization (IVF), to prevent your children from inheriting the same mutation.
Negative with a Variant of Unknown Significance (VUS): This is a result that is still negative for a pathogenic mutation, but you have some genetic variations that the lab does not have enough information to classify as benign (which we ignore) or associated with increased development of cancer (pay attention to). Over time, as more information on these genetic variants is analyzed, the lab will have enough data to reclassify them and contact you. Our experience has been that most of these variants get reclassified as benign (not bad, and therefore ignored). VUS are very common, and doctors treat this result just as they would a negative result, meaning they determine what cancer screening is appropriate based on your age, family history, or other personal risk factors.
Caveats: We are just beginning to understand personalized genomic medicine and translate this information into the risk of disease. We would expect that new genetic variants will be discovered that may affect your risk of cancer or other diseases over time; additional testing (what your provider may call “update testing”) may be recommended. There also may be a change in family history or newer recommendations on how to prevent cancer or other diseases. We recommend you discuss any changes with your doctor on a regular basis to determine if additional screening or medical management would be indicated.
The lab we use has post-test genetic counseling available by telephone, regardless of your results. However, we can also recommend a genetic counselor or a physician to help you assess your risk of cancer.
Remember, most cancers are not related to a known specific hereditary cancer mutation, so you should never neglect age-appropriate screening, taking into account your individualized risk, including family and personal history.
This information is for guidance only. It is not meant to give specific medical advice. Always consult your healthcare provider for appropriate directions.
Yodeah does not provide medical services, make medical referrals or endorse or promote any specific medication, treatment, product or service. Links provided on this website to order test kits are provided solely as a convenience to this website’s visitors. Yodeah is not responsible for the processing of test kits or the provision of test results for any testing service. Yodeah makes no representations regarding the accuracy or efficacy of any testing service.
Yodeah’s mission is to educate and facilitate cost-effective testing for hereditary cancer genetic mutations in the Jewish community, a process known as population-based testing. Yodeah does not give medical advice. We recommend you contact your healthcare professional for any questions about cancer or genetic testing. Genetic testing is not a substitute for visits to a healthcare professional for recommended screenings or appropriate follow-up.